Health professionals agree that breastfeeding is important for long-term child health, and it has also been suggested by policymakers as a way to reduce the risk of poverty and household food insecurity (HFI). But a recent PSI Foundation–funded study has challenged the conventional wisdom regarding breastfeeding duration and HFI, suggesting that it may be more important to focus on other strategies to reduce poverty.
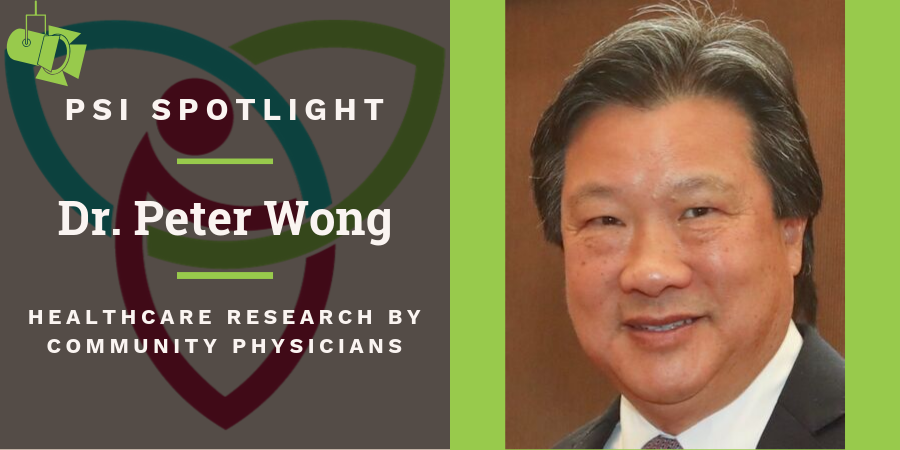
“The benefits of breastfeeding are well recognized, but will it protect families from household food insecurity? Maybe not,” says Dr. Peter Wong, a pediatrician in Toronto.
Because breastmilk substitutes are expensive and could take money away from a household’s food budget, policymakers have suggested that encouraging longer duration of breastfeeding can be one way to decrease the risk of HFI. No research demonstrating the effectiveness of this strategy had previously been done, although studies have shown that the presence of HFI may adversely affect the duration of breastfeeding.
With a PSI Foundation Healthcare Research by Community Physicians grant, Dr. Wong and a team of researchers led by Drs. Patricia Parkin, Jonathon Maguire, Cory Borkhoff and Catherine Birken at TARGetKids!, a research group that focuses on early childhood health, explored this question. A unique research group in Canada, TARGetKids! includes a study population of 10,000 healthy children recruited at community-based practices to provide information about their growth, development and lifestyle to help researchers answer questions about this understudied group.
Dr. Wong and his colleagues surveyed 3,000 families from TARGetKids!, asking questions about breastfeeding duration, household food insecurity and family income. Surprisingly, they did not find an association between breastfeeding duration and HFI, suggesting that shorter duration does not increase the risk of HFI in their study population.
While Dr. Wong notes that the TARGetKids! study group provided access to a large study sample, he also says that the participants were not necessarily reflective of the population where HFI is a pressing concern, which may have influenced the results. Still, the study suggests that breastfeeding on its own may not be enough to help families struggling with poverty and HFI.
“To address household food insecurity, we need a higher level, upstream strategy that addresses more societal problems,” says Dr. Wong. “We need policies that will reduce insufficient income and poor employment. That’s where we’ll make a greater difference.”
Dr. Wong and the team are now planning to examine how breastfeeding and other health-related factors might influence measures of early childhood health, such as nutrition, development and cardiometabolic health. His primary role as a practising pediatrician, as well as his interest in community engagement, public health and epidemiology, gives him unique insight into these types of research questions. “As community physicians, we interact with families and kids on a daily basis, and we have a good appreciation for their health and social challenges,” he says. “We are able to formulate research questions that really have an impact on the health of families and communities.”
And he appreciates that PSI Foundation is supportive of physicians like him who do not have access to the same resources as academic researchers. “Full-time community clinicians have a challenging time competing in the same funding pool as academic researchers,” he says. “PSI Foundation demonstrates that physicians really do care about medical research and about asking questions that address the health of Ontarians.”